1- Mucositis:
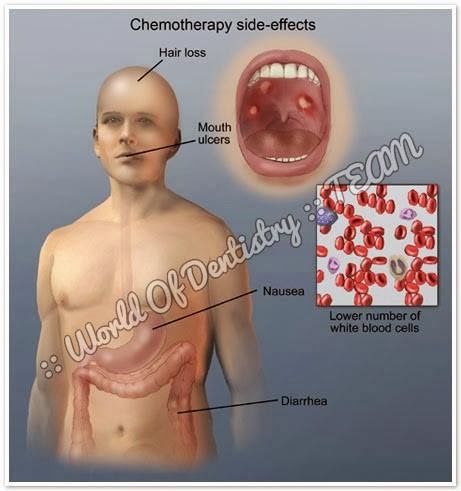
- Mucositis is an inflammatory reaction of the mucosal membranes secondary to antineoplastic treatments such as radiotherapy (in 80% of the cases) and chemotherapy as treatment for solid tumors or lymphomas (in approximately 40-50%, particularly with the cytostatic agent 5-fluorouracil) or as conditioning treatment for bone marrow transplantation (in over 75% of the patients).
- Mucositis is regarded as a manifestation of leukopenia.
- The mechanism by which mucositis develops is not clear, though it is generally attributed to the fact that the oral mucosal cells have a relatively high mitotic rate, thereby establishing them as targets of the action of cytostatic agents.
- Mucositis usually appears 4-7 days after the start of highdose chemotherapy, and is of a self-limiting nature (provided Over-infection does not occur). It in turn disappears 2-4 weeks after the conclusion of cytotoxic chemotherapy.
- The drugs most often associated with the development of mucositis are doxorubicin, bleomycin, fluorouracil and methotrexate.
- Clinically, the condition manifests as erythema, edema or ulceration, with severe pain, bleeding and potential side effects such as xerostomia, the risk of both local (overinfection due to Candida) and systemic infection, malnutrition, fatigue, dental caries and gastrointestinal disorders over time.
2- Oral infections:
The main infectious processes are the following:
1. Bacterial infections: These are usually caused by gram-negative organisms. Signs of inflammation may be masked as a result of the underlying bone marrow suppression; consequently, oral hygiene protocols that reduce microbial colonization of the dentition and periodontium are important during the period of bone marrow suppression.
2. Fungal infections: Bone marrow suppression, oral mucosal lesions and salivary alterations contribute to the development of Candida albicans infection. The most common presentations are pseudomembranous candidiasis, followed by erythematous candidiasis. The treatment of these conditions involves the use of topical and/or systemic antifungal agents (Table 2) complemented with an antiseptic (chlorhexidine). The latter should be used at least 30 minutes before or after nystatin, since the combination of both may prove ineffective. In the case of more severe infections, the recommendation is a systemic antifungal such as fluconazole or ketoconazole.
The efficacy of such treatment is limited, and resistances may appear. In such cases intravenous amphotericin B or itraconazole via the oral route at a dose of 200-400 mg/day tend to be the drugs of choice.
3. Viral infections: In most cases, infections due to herpes simplex virus (HSV), varicella-zoster virus (VZV) and Epstein-Barr virus (EBV) are the result of the reactivation of a latent virus, while infections due to cytomegalovirus (CMV) can result from the reactivation of a latent virus or from a recently acquired virus.
- Infection due to HSV: The severity of the lesions increases drastically with the degree of immune suppression.
The treatment of HSV infection consists of the administration of 400-800 mg of aciclovir via the oral route 5 times a day or of 5-10 mg/kg via the intravenous route every 8-12 hours, for as long as the lesions persist.
- Infection due to VZV: Immune compromised patients may present involvement of several dermatomes, or alternatively the lesions may show a more generalized distribution, generally manifesting several weeks after the interruption of chemotherapy – in contrast to the situation with HSV.
2- Oral infections:
The main infectious processes are the following:
1. Bacterial infections: These are usually caused by gram-negative organisms. Signs of inflammation may be masked as a result of the underlying bone marrow suppression; consequently, oral hygiene protocols that reduce microbial colonization of the dentition and periodontium are important during the period of bone marrow suppression.
2. Fungal infections: Bone marrow suppression, oral mucosal lesions and salivary alterations contribute to the development of Candida albicans infection. The most common presentations are pseudomembranous candidiasis, followed by erythematous candidiasis. The treatment of these conditions involves the use of topical and/or systemic antifungal agents (Table 2) complemented with an antiseptic (chlorhexidine). The latter should be used at least 30 minutes before or after nystatin, since the combination of both may prove ineffective. In the case of more severe infections, the recommendation is a systemic antifungal such as fluconazole or ketoconazole.
The efficacy of such treatment is limited, and resistances may appear. In such cases intravenous amphotericin B or itraconazole via the oral route at a dose of 200-400 mg/day tend to be the drugs of choice.
3. Viral infections: In most cases, infections due to herpes simplex virus (HSV), varicella-zoster virus (VZV) and Epstein-Barr virus (EBV) are the result of the reactivation of a latent virus, while infections due to cytomegalovirus (CMV) can result from the reactivation of a latent virus or from a recently acquired virus.
- Infection due to HSV: The severity of the lesions increases drastically with the degree of immune suppression.
The treatment of HSV infection consists of the administration of 400-800 mg of aciclovir via the oral route 5 times a day or of 5-10 mg/kg via the intravenous route every 8-12 hours, for as long as the lesions persist.
- Infection due to VZV: Immune compromised patients may present involvement of several dermatomes, or alternatively the lesions may show a more generalized distribution, generally manifesting several weeks after the interruption of chemotherapy – in contrast to the situation with HSV.
A number of antiviral agents are used as treatment, depending on the degree of immune suppression of the patient and the resistances to these drugs (Table 2).
- Infection due to CMV and EBV: Lesions produced by CMV are characterized by the presence of multiple mild or moderate ulcerations with irregular margins. The initial lesions appear during the first periods of bone marrow regeneration and are characterized by nonspecific pseudomembranous ulcers covered by a fibrin exudate with a granulomatous base.
- Infection due to CMV and EBV: Lesions produced by CMV are characterized by the presence of multiple mild or moderate ulcerations with irregular margins. The initial lesions appear during the first periods of bone marrow regeneration and are characterized by nonspecific pseudomembranous ulcers covered by a fibrin exudate with a granulomatous base.
At present, ganciclovir is the treatment of choice for acute CMV infection. The risk of EBV infection usually manifests months after the interruption of myeloablative therapy used for transplant conditioning.
3- Neurotoxicity:
- A number of chemotherapeutic agents such as vincristine and vinblastine are able to cause direct neurotoxicity.
- Patients may experience deep and palpitating mandibular pain that tends to subside one week after concluding chemotherapy.
- A number of chemotherapeutic agents such as vincristine and vinblastine are able to cause direct neurotoxicity.
- Patients may experience deep and palpitating mandibular pain that tends to subside one week after concluding chemotherapy.
- A correct anamnesis is required, together with oral exploration and an X-ray study in order to distinguish such pain from pain of pulp origin.
- In some cases, dental hypersensitivity may appear weeks or months after the end of chemotherapy; in these cases, the topical application of fluoride or the use of a desensitizing toothpaste may help lessen the symptoms.
4- Dysgeusia:
- During chemotherapy, patients may experience an unpleasant metallic taste due to diffusion of the chemotherapeutic agent into the oral cavity.
4- Dysgeusia:
- During chemotherapy, patients may experience an unpleasant metallic taste due to diffusion of the chemotherapeutic agent into the oral cavity.
- Dysgeusia as such initially manifests a few weeks after starting cytotoxic treatment, and is generally reversible within a few weeks.
5- Hyposialia and xerostomia:
- Hyposialia, attributable to the effect of chemotherapy upon the cells of the salivary glands, is transient and reversible.
5- Hyposialia and xerostomia:
- Hyposialia, attributable to the effect of chemotherapy upon the cells of the salivary glands, is transient and reversible.
- It appears particularly with the use of adriamycin, and can cause oral functional problems, especially in relation to speech and mastication.
- These patients show alterations in the salivary components, with an increase in the levels of peroxidase and amylase, a reduction in total secreted immunoglobulins A and G, and the presence of the chemotherapeutic drug itself. all these factors favor the development of mucositis.
- As a result, patients should drink abundant water and use sugar-free sweets or chewing gum to increase salivation.
- In more moderate cases, sialogogues such as pilocarpine, bromhexine or bethanechol can be used.
6- Alterations in dental growth and development:
- Unlike radiotherapy, which only affects the cells within the irradiated zone, chemotherapy has a systemic effect.
- As a result, the developing odontogenic cells are susceptible to chemotherapy, even when far removed from the tumor site.
- As a result, patients should drink abundant water and use sugar-free sweets or chewing gum to increase salivation.
- In more moderate cases, sialogogues such as pilocarpine, bromhexine or bethanechol can be used.
6- Alterations in dental growth and development:
- Unlike radiotherapy, which only affects the cells within the irradiated zone, chemotherapy has a systemic effect.
- As a result, the developing odontogenic cells are susceptible to chemotherapy, even when far removed from the tumor site.
7- Bleeding tendency:
- Bleeding is due to alterations resulting from thrombocytopenia (in turn a consequence of bone marrow aplasia).
- Clinically, patients my present petechiae, ecchymosis, hematomas or diffuse bleeding.
- Rinses with 0.12% chlorhexidine avoid overinfection and can help eliminate the traces of blood, though caution is required in order not to alter the clots, since this could lead to further bleeding.
8- Osteonecrosis:
- Osteonecrosis of the jaw (ONJ) is observed in patients treated with bisphosphonates (BPs).
- These drugs inhibit bone resorption and are administered via the intravenous route as treatment in application to bone metastases in cancer patients, in malignant hypercalcemia (tumorinduced hypercalcemia), or in patients with multiple myeloma – affording improved survival and quality of life.
- Although much less commonly, ONJ has also been observed in patients receiving treatment with oral bisphosphonates (used for the prevention and treatment of osteoporosis and in certain bone conditions such as Paget’s disease).
- The intravenous BPs most associated with ONJ are zoledronic acid (Zometa®) and pamidronate (Aredia®).
- Clinically, ONJ is typically characterized by pain (progressive and sustained, and sometimes requiring important analgesic doses to secure control – the patient being asymptomatic in the early stages).
- Since the treatment of ONJ is often unsatisfactory, management should aim to afford pain relief, control soft tissue and bone infection, and avoid or reduce the progression of bone necrosis.
- Clinically, ONJ is typically characterized by pain (progressive and sustained, and sometimes requiring important analgesic doses to secure control – the patient being asymptomatic in the early stages).
- Since the treatment of ONJ is often unsatisfactory, management should aim to afford pain relief, control soft tissue and bone infection, and avoid or reduce the progression of bone necrosis.
-----------------------------------
This Article has been Edited by :: World Of Dentistry :: TEAM
For any suggestions please don't be hesitate to feedback us
:: World Of Dentistry :: TEAM
This Article has been Edited by :: World Of Dentistry :: TEAM
For any suggestions please don't be hesitate to feedback us
:: World Of Dentistry :: TEAM