- Pulp capping:It is a term is derived from the name pulp cap which means trying to sterilize the damaged tooth area as well as one can, followed by stopping the bleeding and placing the right filling material on it.
- The precaution being that teeth that are already abscessed should never be pulp-capped – this is done to those teeth where the nerve is irritated but still alive and healthy enough to repair themselves given a chance to do so.
- Pulp capping gives it a chance by getting out the decayed portions and the bacteria then putting a clean dressing on it with the filling.
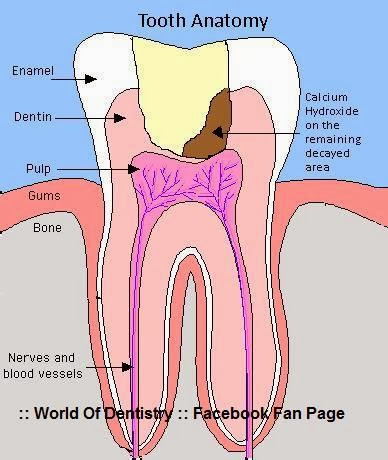
- After eliminating the wounded dental tissues of a carious tooth, the next step is usually filing the cavity with a suitable restoring material. When pulpal tissue is exposed it gets contaminated by bacteria and mostly these are the conditions that warrant the clinician to perform pulp capping. When performing this procedure, the degree of the pain and the pulpal size exposure are considered.
- Capping Materials:
- Calcium Hydroxide is the best possible capping material known till now.
- Advantages of Calcium Hydroxide:
1-It's alkaline PH (11) ... Giving more chances to healing of inflamed tissues.
2-Amazing bio-compatibility with pulpal tissues.
3-It's antibacterial Abilities (Bacterio-static).
4-It's ease of application.
5-Availability.
6-It's proven Abilities to dentine bridging for regeneration of healing dentinal tubules in the pathosed dentine pulp complex.
- Disadvantages of Calcium Hydroxide:
1- Associated with primary tooth resorption
2- May dissolve after one year with cavo-surface dissolution.
3- May degrade during acid etching
4- Degrades upon tooth flexure
5- Marginal failure with amalgam condensation
6- Does not adhere to dentin or resin restoration.
- NOTE:
Calcium hydroxide was originally introduced to the field of endodontics by Hermannin:: 1920 as a pulp-capping agent.
- Many studies have showed that direct pulp capping with MTA Is as successful ...
- Placing the restoration directly without capping on a pinpoint exposed pulp:
1- Severe sensitivity the patient will suffer.
2- Failure of restoration.
3- Irreversible pulpal tissue damage that will require endodontic treatment.
- The Pulp Capping is two Types: Direct and Indirect Pulp Capping:
- Direct Pulp Capping:
- The exposed pulp is directly covered. This works best when the exposure is not infected - for example a traumatic exposure caused by slipping with the drill.
- If the pulp becomes exposed while removing soft infected dentine, the chances are that the pulp will be infected also, and a direct pulp cap will fail (that is, an irreversible pulpitis will develop).
- Placing the restoration directly without capping on a pinpoint exposed pulp:
1- Severe sensitivity the patient will suffer.
2- Failure of restoration.
3- Irreversible pulpal tissue damage that will require endodontic treatment.
- The Pulp Capping is two Types: Direct and Indirect Pulp Capping:
- Direct Pulp Capping:
- The exposed pulp is directly covered. This works best when the exposure is not infected - for example a traumatic exposure caused by slipping with the drill.
- If the pulp becomes exposed while removing soft infected dentine, the chances are that the pulp will be infected also, and a direct pulp cap will fail (that is, an irreversible pulpitis will develop).
- Although Calcium Hydoxide has been proven successful for many years, MTA (Mineral Trioxide Aggregate) is fast becoming the material of choice for direct pulp caps. MTA is however very expensive.
- Indirect Pulp Capping:
- The pulp is not exposed - a layer of infected dentine is deliberately left, rather than expose the pulp.
- Indirect pulp caps, when done correctly, are more successful at maintaining long-term vitality than direct ones.
- It is not currently (2010) known whether it is necessary to "go in again" after a couple of months for further caries removal.
---------------------------
This Article has been Authored By :: World Of Dentistry :: TEAM
For any questions and Suggestions please don't be hesitate to feedback us.
Yours,
:: World Of Dentistry :: TEAM
- Indirect Pulp Capping:
- The pulp is not exposed - a layer of infected dentine is deliberately left, rather than expose the pulp.
- Indirect pulp caps, when done correctly, are more successful at maintaining long-term vitality than direct ones.
- It is not currently (2010) known whether it is necessary to "go in again" after a couple of months for further caries removal.
---------------------------
This Article has been Authored By :: World Of Dentistry :: TEAM
For any questions and Suggestions please don't be hesitate to feedback us.
Yours,
:: World Of Dentistry :: TEAM